Overview
Parkinson’s Disease patients often experience Freezing of Gait (FoG), sudden moments where their feet feel “stuck” to the ground, especially on flat surfaces. Research shows that continuous motion (like climbing stairs or cycling) reduces FoG, and even 3D illusions of stairs can help patients regain mobility.
This project explored how Mixed Reality (MR) could transform flat surfaces into stair-like illusions, creating a transformative experience that helps patients move more freely.
The Problem
• FoG affects up to 70% of advanced Parkinson’s patients, causing falls, loss of independence, and reduced quality of life
• Physical interventions (painting 3D illusions on floors) have shown success but are limited to controlled indoor environments and lack portability.
• There is a need for an adaptive and discreet solution that works in everyday environments.
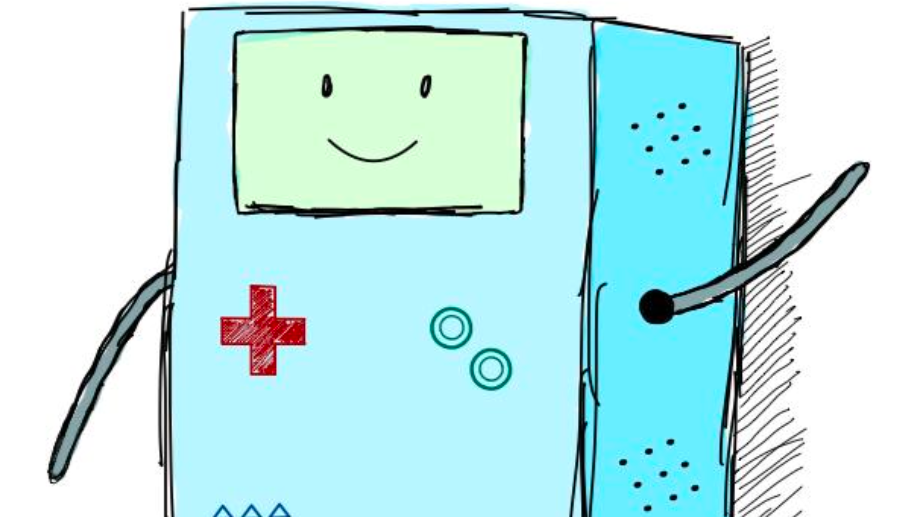
The Solution
I proposed a Mixed Reality headset application that dynamically overlays 3D images of stairs and textured surfaces onto the user’s walking path. By tricking the brain into perceiving continuous motion, the system aims to reduce freezing episodes and increase the user's confidence.
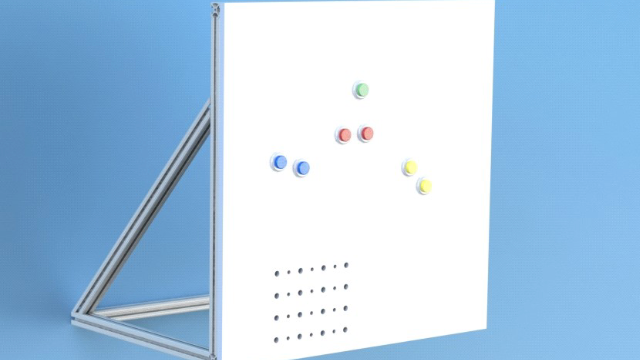
Hardware
Initial prototypes targeted the Magic Leap headset, with expansion planned for Oculus and HTC devices.
Software
Developed in Unity, with the Lumin SDK for Magic Leap to leverage native performance and responsiveness.
Interaction
Patients see flat floors transformed into stair-like, triggering smoother, more natural steps.
Design Approach
This work was conducted under MIT’s Humanistic Co-Design Initiative, ensuring solutions were developed with and for people with disabilities.
Research & Co-Design
Narrative reviews, semi-structured interviews with clinicians and patients, and creation of personas to capture pain points.
Concept Development
Applied the Design Innovation (DI) framework — Discover, Define, Develop, Deliver — to refine opportunity statements into a feasible MR concept.
Validation
Conceptual models were reviewed with therapists; early user acceptance testing (UAT) was planned with both able-bodied and PD participants.
Impact
• Provided a novel digital alternative to physical visual cues, making therapy portable and adaptable to daily life.
• Showcased how emerging technologies (AR/VR/MR) can integrate into physical therapy and long-term care.
• Recognized with a special award in the National Olympiad for Scientific Creativity, validating both technical and social value.
Next Steps
Future iterations would expand into:
• Prototype testing with PD patients.
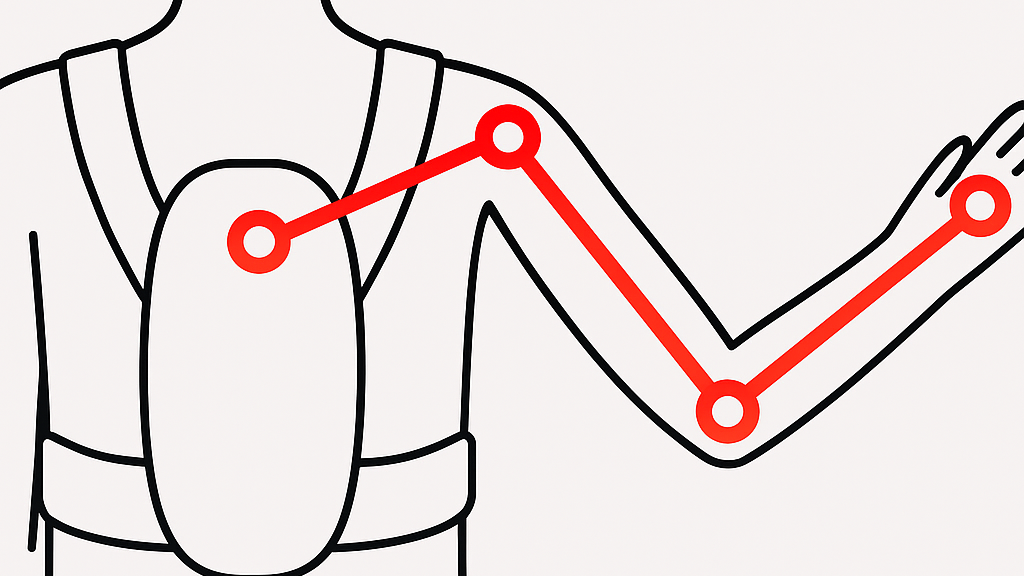
• Integration of sensor data (accelerometers, gait trackers) for adaptive feedback.
• Exploring partnerships with healthcare providers for clinical deployment.